Snapshot
- Nearly every sexually active person will acquire HPV at least once in their life.
- HPV infections can lead to cancers in the cervix, vulva, vagina, penis, anus, and throat and genital warts.
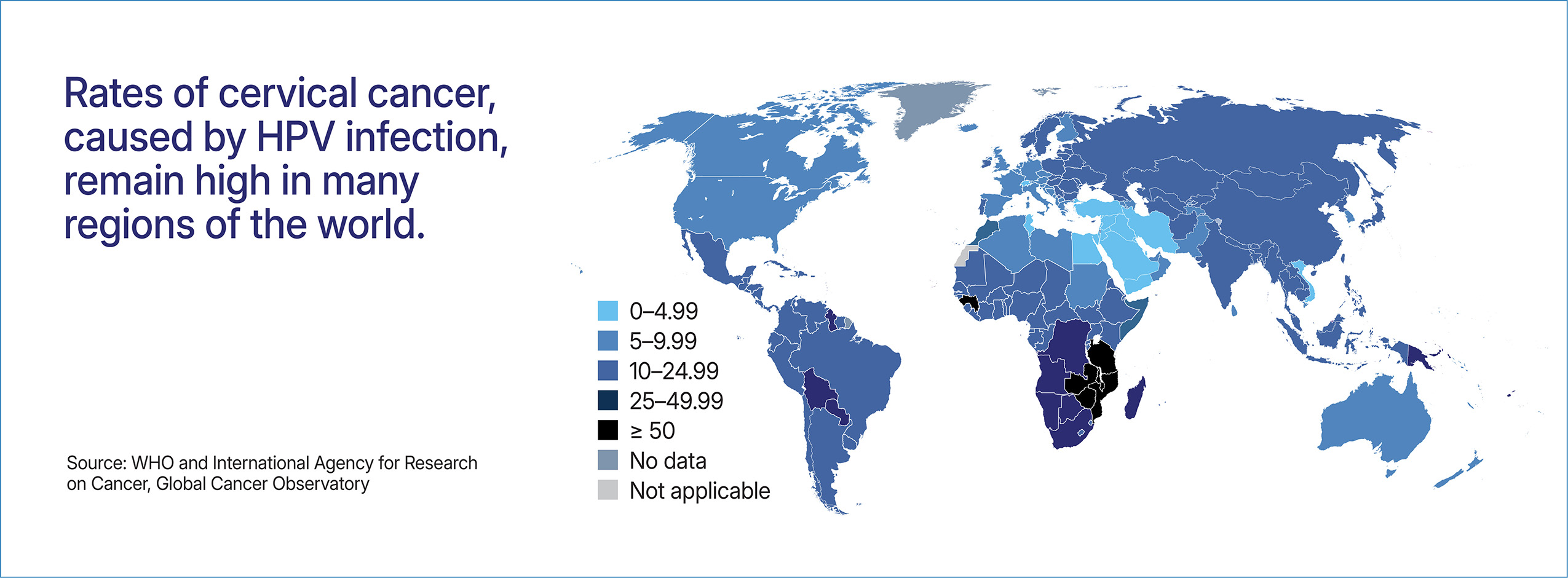
- HPV is the leading cause of cervical cancer, leading to 350,000 deaths every year and impacting low-and middle-income countries.
- Nearly a quarter of women in Sub-Saharan Africa have cervical cancer related to HPV.
- Early detection of HPV infections is critical, because it allows providers to treat precancerous lesions before symptoms appear.
- Vaccines to prevent HPV related cancers and genital warts have been available since 2006. Today these vaccines reach about 1 in 5 girls worldwide.
Key Challenges
- Vaccines have been available for nearly 20 years, yet coverage remains inadequate.
- HPV-related cancer screening programs are limited, leading to missed opportunities to treat pre-cancers and cancers.
HPV Advocacy Needs
- Are vaccines available to prevent HPV? Yes. Vaccines are available to prevent HPV related cancers and genital warts but are expensive.
- Are tests available to detect HPV? Yes, HPV tests, that include self-collected vaginal swabs.
- How is HPV detected? While HPV tests are available, cancer screening, including anal and cervical, are primarily used to detect HPV-related cancers.
- Can HPV be treated? While HPV cannot be treated, HPV-related cancers can be treated.
Vaccines
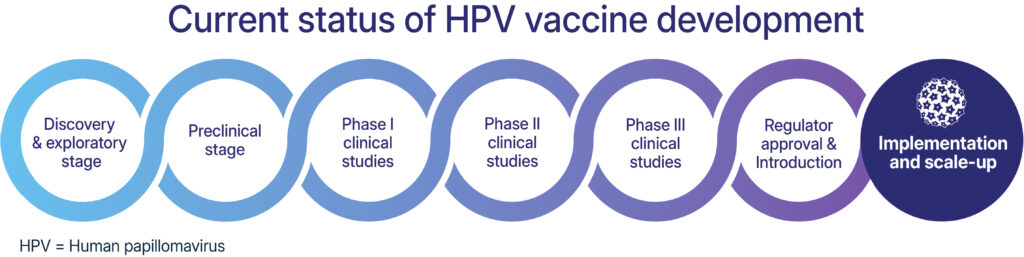
Preventive HPV vaccines became available in 2006, and by mid-2024 had been introduced into routine immunization programs in 139 countries. In 2023, an estimated 27% of adolescent girls and 7 percent of adolescent boys worldwide had received a first dose of vaccine against HPV. To achieve the goals of the Global Strategy for cervical cancer elimination, 90 percent of girls will need to receive vaccines.
While HPV vaccines were initially administered as a three-dose series, WHO now endorses a single dose for those who receive the vaccine between the ages of 9-20. This change reduces costs and simplifies the logistics of administering the vaccine. Immunocompromised individuals, including people living with HIV, should receive at a minimum two doses and where possible three doses.
The World Health Organization currently licenses six HPV vaccines that each protect against 2 or more strains of HPV. Research is still needed to develop vaccines that offer protection against additional strains, as well as therapeutic vaccines, which are under development to help in the treatment of HPV related cancers and pre-cancers.
Advocacy Needs
- Advocates should continue to press countries to include HPV vaccination in routine immunization programs, and press manufacturers and donors to ensure sufficient vaccine supply.
- Additional evidence is needed to support the shift to a one-dose schedule and to show benefits of vaccination for boys and men.
- Implementation research is needed to identify additional ways to improve HPV vaccine acceptability and uptake.
Diagnostics
Historically, cervical cancer has been detected using the Papanicolaou (Pap) test, which examines cervical cells for abnormalities. More recent tests can provide primary screening for HPV in cervical cells, reducing the need for Pap tests and helping to identify pre-cancerous cells before symptoms appear. Samples for these newer diagnostics, which rely on molecular testing, may be collected by a provider or self-collected with a vaginal swab, and then sent to a laboratory for processing. Like other molecular-based tests, however, these HPV tests may be difficult to implement in resource-limited settings.
There are currently no tests available to detect HPV in parts of the body other than the cervix. Some providers conduct anal Pap tests or screening to detect HPV-related anal cancers.

Advocacy Needs
- Affordable, user-friendly, effective, and rapid point-of-care tests are needed to identify HPV infections and HPV-related cancers.
Treatment
There is no treatment for HPV infection. However, providers can screen for and treat precancerous lesions to prevent them from progressions to cancer. Lesions may be removed surgically or by burning or freezing them. Additionally, treatments are available for HPV-related cancers including cervical cancer.